Respiratory physiotherapy in MND - what is it and why is it so important?
Motor neuron disease (MND) affects the nerves that support movement, including those that control the breathing muscles, causing them to weaken, paralyse and waste. Weak respiratory muscles impact the ability to breathe in and ventilate the lungs, and to breathe out making it difficult to cough and clear the airways.
Initially, breathing symptoms may show as shortness of breath or fatigue with exertion (walking or climbing stairs), then with mild exertion (speaking, lying down) and eventually most of the time.
The good news – there are a vast range of ways respiratory physiotherapy can help manage these symptoms, and even prolong duration and quality of life!
Positioning and mobility – to keep moving and exercising in ways someone enjoys is the best way to facilitate a deep breath in and good ventilation. This looks different for everyone with MND - it might be going for a short walk, cycling, standing up as tall as possible or maintaining good posture when sitting. Positioning in bed is also important as people with MND often feel short of breath when lying flat. Good head control and posture is also vital to keep the airways open.
Rib cage and thoracic mobility – like all other joints and muscles in the body, those surrounding the rib cage and spine will stiffen up if not used. Physiotherapy exercises can keep these areas as free as possible so that they are ready to expand for a big breath in.
Insufflation exercises – techniques like the active cycle of breathing technique and breath stacking can assist ventilation. Equipment can be used to support this, such as incentive spirometry (this provides a visual prompt as to how much air is coming in) or putting our hands on to feel the rib cage expand.
Insufflation exercises
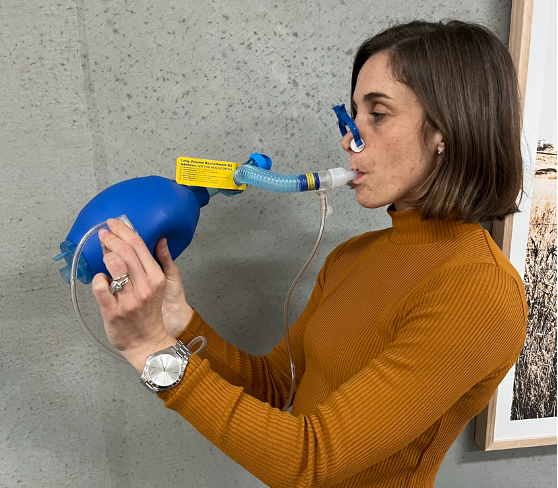
LVR Kit
Lung volume recruitment (LVR) – this is a simple technique using a LVR kit to support a bigger breath in when the person’s inspiratory muscles can no longer do it for them. It helps to open collapsed airways to increase gas exchange and keep the lungs healthy by preventing an infection in the underinflated areas.
Exsufflation exercises – maintaining a short, sharp, strong breath out is important to clear irritants, bugs and food from the airways. Expiratory muscle exercisers such as the Power Breathe can do this by providing the right amount of resistance when breathing out (as a dumbbell would be used for a bicep curl), to maintain muscle strength. Different supported cough and huff techniques can also be tried.
Manual assisted cough – when the expiratory muscles are no longer strong enough to create an effective cough, an assisted cough can be taught by applying a firm pressure to either the diaphragm or the abdominal contents to increase the pressure require to force the air out. This combined with assisted insufflation can make a cough much stronger and more productive.
Cough assist machine
Cough assist machine – some people find the use of a machine to help them cough beneficial. A mouthpiece or face mask is used to facilitate a big breath in and then draw a quick breath out triggering a cough. Respiratory physios can determine if this machine is likely to be beneficial, and if so, what the best settings are for each individual.
Non-invasive ventilation (NIV) – using NIV for more than 4 hours per day leads to slower disease progression, improved sleep, improved quality of life, reduced fatigue and increase survival times. Respiratory physiotherapists can work with the Victorian Respiratory Support Service (VRSS) to determine the best time to start NIV and the optimal settings.
Secretion/sputum management – respiratory physiotherapy techniques can help with secretion management during a chest infection, and towards the end stages of MND. In addition to hands on techniques like percussions, vibrations and postural drainage, prescribing equipment like nebulisers (to loosen secretions so they shift more easily) or suction units (to help draw the secretions out) can help.
Difficulty getting a breath in, clearing secretions and fear of choking can be scary for people living with MND. You do not have to navigate this alone, and we are here to help. For more information on our neurorespiratory physiotherapy service and how it might help you or someone you know please call us on 42070279 or email zoe@neurophysiogeelong.com.au